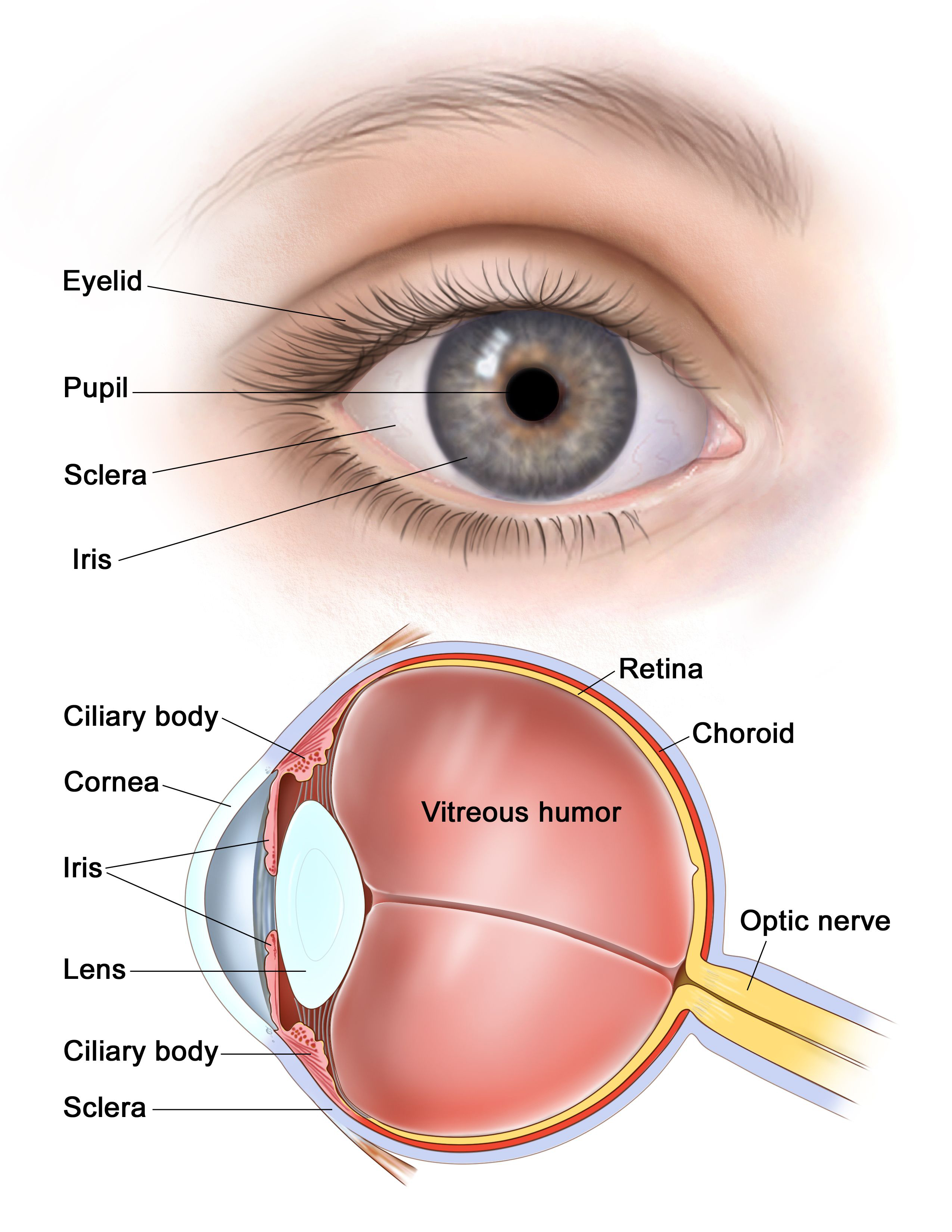
What is Cornea?
The cornea is the transparent part of the eye that covers the front portion of the eye. It covers the pupil (the opening at the center of the eye), iris (the colored part of the eye), and anterior chamber (the fluid-filled inside of the eye). The cornea’s main function is to refract, or bend, light. The cornea is responsible for focusing most of the light that enters the eye.
The cornea tends to repair itself quickly from minor abrasions. However, deeper abrasions may cause scars to form on the cornea, which causes the cornea to lose its transparency, leading to visual impairment. Consult Dr. Sonia Maheshwari Kothari, Cornea Specialist in Mumbai at Clear Sight Eyecare & Laser Centre Clinic in Ghatkopar East, for Cornea Treatment.
Corneal Pathologies
A. KERATOCONUS
WHAT IS KERATOCONUS?
Keratoconus is a bilateral asymmetric disorder of the eye where there is gradual thinning and bulging of the central portion of the cornea forwards in a conical shape. It is associated with significant visual problems like blurring and distortion of vision, increased sensitivity to light etc.The cornea is responsible for refracting (focussing) accurately most of the light coming into the eye. Therefore, abnormalities of the cornea severely affect the way we see the world making simple tasks, like driving, watching TV or reading a book difficult.
WHAT CAUSES KERATOCONUS?
The cause of keratoconus is still unknown despite our long experience with it. There has been no shortage of speculation or study and numerous theories have been proposed.One scientific view is that keratoconus is developmental (i.e., genetic) in origin. This suggests that it is the consequence of an abnormality of growth, essentially a congenital defect. Another view is that KC represents a degenerative condition. Still a third view is that KC is secondary to some disease process. A less widely held hypothesis suggests that the endocrine system may be involved. This idea gained credence from the usual appearance of the disease because it is generally first detected at puberty when a lot of hormonal changes usually occour in the body.Risk factors are genetic predisposition,family history,contact lens wearers, chronic allergy, vernal keratoconjunctivitis, eye rubbing,ocular disorders like retinitis pigmentosa, retinopathy of prematurity, connective tissue disorders etc.
DOES IT CAUSE COMPLETE BLINDNESS?
No, very few if any persons suffer from total blindness from keratoconus alone. But in severe cases, one’s vision can be significantly impaired and normal everyday activities may be difficult. However with the currently available treatment options most patients retain useful vision enabling them to lead normal productive lives.
HOW TO TREAT IT?
There are a number of treatment modalities available for the management of keratoconus. It depends on the signs and symptoms and the stage of the disease. For mild to moderate cases, glasses and soft contact lenses are prescribed as the first line of treatment. As the disease progresses the quality of vision deteriorates and soft contact lenses fail to provide satisfactory vision due to increase in the irregularities of the corneal surface. The following can be done for advanced progrssive cases:
1. Custom soft contact lenses
Wide range of fitting parameters are available for a customized fit and are larger in diameter than regular soft lenses for greater stability on a keratoconic eye.
2. Rigid gas permeable contact lenses
These are preferred for highly irregular corneal surface. These lenses vault over the cornea, masking its irregular shape with a smooth, uniform refracting surface to improve vision.
3. Hybrid contact lenses
These lenses with their wide variety of fitting parametersare a combination of a rigid centre with a soft peripheral skirt. The centre of the lens is highly permeable to oxygen and it fits over the central conical portion of the cornea to provide comfortable and clear vision.
4. Piggyback contact lenses
it includes one soft contact lens which is placed over the cornea for better comfort and then a rigid contact lens is placed over the soft lens to provide a smooth refracting surface. This combination thus improves the overall fit and comfort of the patient.
5. Semi-scleral and scleral lenses
they are large in size with their periphery touching the sclera which is the white portion of the eye. They put less pressure on the cone area and provide a better stability and comfort.
6. Intacs
These are transparent,rigid arc shaped ring segments made of inert non-toxic material which are positioned surgically inside the cornea. It is mainly used in cases of decentred cones to regularise and reshape the corneal surface. It reshapes the cornea without removing any tissue preserving the biomechanical integrity of the cornea. This procedure intends to flatten the central cornea both to decrease the cone in keratoconus and to achieve myopic correction without compromising the biomechanical integrity of the cornea. The patients will still require glasses or contact lenses after this but the flattening achieved with this procedure helps in a better visual rehabilitation of the patient.
7. Corneal cross-linking
It helps in halting the progression of the disease. It is being widely used nowadays in the management of the disease with promising results. In this procedure, cornea is saturated with riboflavin eye drops which is followed by exposure to ultraviolet light rays. There are various protocols available to carry out this procedure, selection of which depends upon the corneal parameters (as determined by corneal topography) and the grade of keratoconus. This helps in providing strength to the cornea and prevents further corneal bulging by forming new bonds between the collagen fibrils. It significantly reduces the need to carry out a corneal transplant procedure. It can be combined with intacs and other laser procedures done for keratoconus to achieve better results and to improve stability over a long period of time.
8. Corneal transplant
It is the treatment of choice in patients with advanced progressive disease with corneal scarring and extreme thinning. It is generally reserved as the last treatment option when all other procedures fail. In this procedure a donor cornea is used to replace the patient’s diseased cornea and held in place with the help of corneal sututres. It takes a few months for the stabilization and visual recovery. It is associated with complications such as graft rejection, infection,interface haze etc.
LASER PROCEDURES IN KERATOCONUS:
Topography- guided photorefractive keratectomy (TPRK) followed by corneal collagen crosslinking.
WHAT IS TPRK?
The procedure uses a customized excimer laser treatment guided by topographic map obtained preoperatively. This is done on the Schwind Amaris 1050RS platform which enables a very fast procedure with speedy recovery.
After Laser ablation , the corneal collagen crosslinking is carried out and then a bandage soft contact lens in placed over the eye. This bandage soft contact lens is typically removed after 48 hours which is time taken for the cornea to heal.
WILL TPRK HELP TO REDUCE MY GLASS POWER AFTER SURGERY?
TPRK is primarily done to reduce the irregular astigmatism which is present in keratoconus and not necessarily to improve your distance vision. The goal is to improve your corneal shape in order to improve the quality of your vision with glasses or contact lens.
CAN TPRK BE DONE FOR ALL KERATOCONUS PATIENTS?
No, only patients with early to moderate grade keratoconus with a preoperative thinnest corneal thickness of 450 microns are suitable candidates.
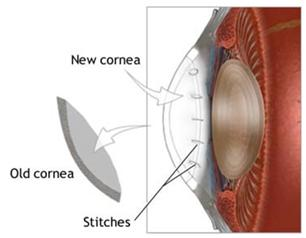
B. CORNEAL TRANSPLANT
WHAT IS A CORNEAL TRANSPLANT?
With corneal transplants, scarred or damaged tissue is replaced with healthy donor tissue. Corneal transplants either replace the whole cornea (standard full thickness known as Penetrating Keratoplasty) or individual layers (partial thickness known as DSAEK, DMEK and DALK). The type of transplant performed depends on the prior condition and extent of the damage.
INDICATIONS FOR FULL THICKNESS CORNEAL TRANSPLANTS
- Advanced keratoconus with severe scarring
- Severe Herpetic scarring
- Full thickness traumatic injury
INDICATIONS FOR DSAEK AND DMEK
- Fuchs’ dystrophy
- Corneal failure after cataract, glaucoma or retinal surgery
- Endothelial failure or rejection of a full thickness transplant
INDICATIONS FOR DALK
- Keratoconus, corneal scarring & pellucid marginal degeneration
- Stromal Corneal Dystrophies
- A healthy endothelium (the innermost layer of the cornea)
HOW DO I KNOW IF I WOULD BENEFIT FROM A CORNEAL TRANSPLANT?
A corneal transplant is normally indicated once your damaged cornea interferes with your ability to do activities important to you or is causing significant constant pain not treatable by other means.
HOW IS THE SURGERY PERFORMED?
Corneal transplants are generally done under local anaesthetic. With full thickness transplants, the damaged cornea is removed through a process called trephination and replaced with a donor cornea. The transplant is then secured using tiny stitches about 1/3 the thickness of a human hair. Partial thickness transplants replace only certain layers, leave the rest intact and use fewer stitches. On treatment day, you will be instructed to arrive at the hospital about 1.5 hours in advance and the surgery will take approximately 30 minutes. No overnight hospital stay is required.
WHAT ARE THE POSSIBLE COMPLICATIONS ?
The success rate of corneal transplants has drastically improved in the last 30 years. Today, the overall success rate is above 85%. However, it can vary from 50% to 95% depending on the condition being treated. Dr. McCarthy will go over your individual case with you. Corneal transplants remain a serious surgery with certain risks that you should be aware of. The primary risks are rejection and infection which are minimized with the use of antibiotic and steroid drops. Other less common complications include bleeding, swelling, glaucoma and retinal detachment. Fortunately, the majority of complications are treatable and have good outcomes.
HOW LONG IS HEALING TIME ?
Healing time is different for everyone. You can expect to have moderate discomfort, irritation and redness for up to 3 weeks. Best possible vision is achieved once wounds have fully healed and stitches removed. Healing of a full thickness transplant can take up to 1 year. Visual improvement with DMEK and DSAEK usually occurs in a few weeks.
WHAT DO I NEED TO DO BEFORE AND AFTER SURGERY ?
You should ensure that you understand all instructions provided. You will start taking antibiotic drops 3 days prior to surgery and continue until the bottle is empty. You will also take steroid drops that will be gradually reduced over time to 1 drop per day, but you will likely continue permanently. It is essential to take your drops as prescribed to maintain function of the transplant. After surgery you should avoid any heavy lifting and strenuous activity for 1 month.
For more information & consultation on Cornea Specialist in Mumbai, visit Clear Sight Eyecare & Laser Centre at Ghatkopar East or contact us on 80978 09788 or simply fill in your name and number & one of our team member will get in touch with you soon. Our team of experts along with Dr. Sonia Maheshwari Kothari, Ophthalmologist Eye Surgeon & one of the Best Eye Specialist in Mumbai, will help you out in understanding your problem and guide you through every stage of your treatment. For Clinic direction click here
