LASIK surgery is one of the most popular procedures for correcting refractive vision problems such as myopia, hyperopia, and astigmatism. While LASIK has proven to be a safe and effective treatment for many patients, not everyone is an ideal candidate for the surgery. A thorough pre-surgical evaluation is critical, and several technical parameters must be assessed before determining a patient’s suitability for LASIK. One advanced diagnostic tool used in this process is the Pentacam test, which provides a detailed analysis of the cornea, playing a crucial role in ensuring the surgery’s safety and success. Let’s dive into these technical parameters in detail.
Corneal Thickness
The thickness of your cornea is one of the most important factors in determining whether LASIK is a safe option. LASIK involves removing a small amount of tissue from the cornea to reshape it and correct vision. If the cornea is too thin, there might not be enough tissue left after surgery, which can lead to complications such as corneal ectasia, a progressive thinning and bulging of the cornea.
- Pentacam Test: The Pentacam test is essential for accurately measuring corneal thickness and providing a 3D map of the corneal structure. It helps surgeons evaluate whether there’s sufficient corneal thickness for the procedure.
- Standard Requirement: A corneal thickness of at least 500 microns is typically required.
- Safety: The surgeon must ensure there is enough corneal tissue remaining post-surgery to maintain corneal strength and integrity.
Corneal Topography
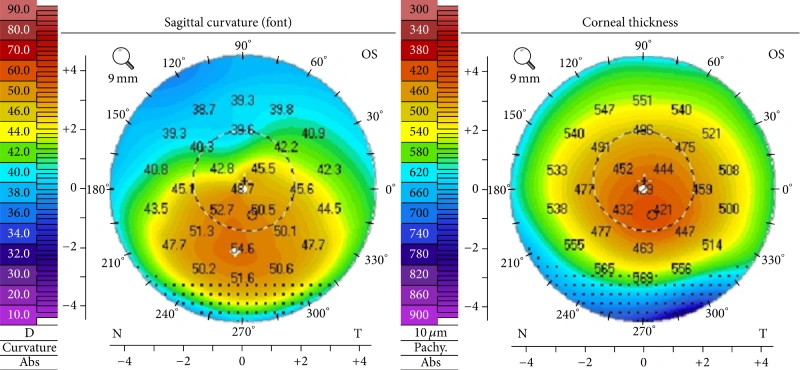
Corneal topography is a detailed map of the surface of the cornea. This helps the surgeon understand the shape and contour of the cornea and detect irregularities such as astigmatism or keratoconus (a condition where the cornea thins and bulges).
- Pentacam Test: The Pentacam provides high-definition corneal topography, offering a detailed view of the corneal curvature, thickness distribution, and even early signs of keratoconus. This ensures the surgeon can detect any irregularities that might disqualify a patient from LASIK.
- Irregularities: Detecting abnormalities in the corneal shape can help prevent complications. For example, patients with keratoconus are not suitable for LASIK.
- Personalization: Corneal topography helps the surgeon create a customized treatment plan based on the patient’s unique corneal structure.
Pupil Size
Pupil size is a critical factor in LASIK surgery, especially when it comes to night vision. Patients with larger pupils may experience more visual side effects after surgery, such as halos, glare, or starbursts, particularly in low-light conditions.
- Night Vision Concerns: Larger pupils increase the risk of post-surgery visual disturbances, especially in dim environments.
- Customized Laser Coverage: The laser treatment must be customized to cover the pupil area effectively under all lighting conditions.
Tear Film and Dry Eye Condition
A healthy tear film is necessary for maintaining eye comfort and vision clarity. Patients with dry eye syndrome may face complications after LASIK, as the surgery can sometimes worsen dry eye symptoms.
- Pre-Surgery Assessment: Tear film tests, such as the Schirmer test, are conducted to evaluate tear production.
- Post-Surgery Impact: Addressing dry eye issues before surgery can help reduce post-operative discomfort and visual fluctuations.
Prescription Stability
LASIK surgery reshapes the cornea based on your current prescription. If your prescription has been fluctuating, it may not be the right time to undergo surgery.
- Requirement: Surgeons generally require a stable prescription for at least one year before LASIK.
- Long-Term Results: A stable prescription ensures that the surgery provides lasting results and reduces the likelihood of needing corrective lenses again in the future.
Corneal Curvature
The curvature of the cornea, also known as keratometry, is an important measurement taken before LASIK surgery. It helps determine the overall shape of the cornea and whether it falls within the acceptable range for surgery.
- Pentacam Test: The Pentacam is particularly useful here as it measures corneal curvature with extreme precision. This helps ensure the cornea is suitable for reshaping during LASIK.
- Normal Curvature: The corneal curvature needs to be within a certain range to ensure that the laser can reshape it properly.
- High Curvature: Patients with abnormally steep or flat corneas may not be suitable for LASIK and might need alternative procedures.
Age
Age plays a significant role in determining LASIK candidacy. While LASIK is generally performed on adults, age-related changes in the eyes, such as presbyopia (the need for reading glasses), can affect the outcome of the surgery.
- Ideal Age Range: Most LASIK candidates are between 18 and 40 years old, with a stable prescription.
- Presbyopia Consideration: Patients over 40 may require additional corrective procedures or alternatives to address age-related vision changes.
Corneal Healing Response
Before LASIK, the surgeon must evaluate how well your cornea is likely to heal after surgery. A good healing response is essential for the success of the procedure.
- Pentacam Test: The Pentacam’s advanced imaging helps predict the healing response by providing in-depth analysis of corneal thickness and health.
- Healing Tests: Surgeons may assess factors like corneal thickness, tear production, and any history of eye conditions to predict healing ability.
- Reduced Healing Capacity: If a patient has a compromised healing ability due to previous eye conditions, they may not be an ideal candidate for LASIK.
Eye Health
Overall eye health is a vital parameter in determining suitability for LASIK. Conditions such as cataracts, glaucoma, or retinal diseases can disqualify a patient from undergoing LASIK.
- Pre-Existing Conditions: Any underlying eye conditions must be addressed or stabilized before surgery.
- Comprehensive Exam: A complete eye exam, including tests for eye pressure, retina health, and lens clarity, is performed to ensure the patient is a good candidate for surgery.
Corneal Reflex and Dominant Eye
Surgeons may test for corneal reflex and assess the dominance of each eye before LASIK. Understanding which eye is dominant helps guide the laser reshaping process and ensures that both eyes are properly balanced after surgery.
- Corneal Reflex Test: This test assesses the eye’s response to stimuli, helping the surgeon plan for accurate corneal reshaping.
- Eye Dominance: Knowing the dominant eye can aid in achieving optimal results, especially if the patient has one eye that naturally performs better than the other.
Pentacam Test: A Crucial Tool in LASIK Preparation
Throughout the evaluation process, the Pentacam test plays a crucial role in determining LASIK candidacy. By providing a comprehensive, 3D analysis of corneal thickness, curvature, and topography, the Pentacam helps ensure that the procedure will be both safe and effective. It allows surgeons to detect potential issues that might disqualify a patient from LASIK, such as early-stage keratoconus, thin corneas, or abnormal corneal shapes. This detailed data enables the surgeon to create a customized treatment plan tailored to each patient’s unique eye structure.
If you’re considering LASIK, it’s essential to consult with an experienced eye specialist. Dr. Sonia, a leading expert in LASIK surgery, provides personalized evaluations and care. To determine whether you are a suitable candidate for LASIK, schedule your appointment today with Dr. Sonia for a comprehensive assessment and individualized treatment plan.

